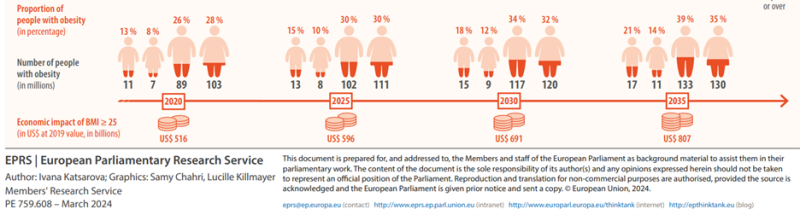
Obesity is no longer a looming crisis – it’s a present and escalating public health emergency across Europe. More than half of EU adults are now overweight, and nearly one in five live with obesity. Since 1975, obesity rates in the WHO European Region have surged by over 130%, and no EU country is on track to meet the WHO’s target of halting obesity at 2010 levels by 2025. Europe could see over half its population living with obesity by 2030, with some Member States nearing 90% overweight or obese. This trajectory threatens to overwhelm healthcare systems, deepen health inequalities, and erode economic resilience. With these projections and given obesity’s strong role as a significant driver of cardiovascular disease, coordinated action from EU institutions in partnership with industry is essential to curb this public health crisis.
Public health must evolve from treatment to prevention, leveraging tools that make healthy choices easier and more appealing. Despite decades of awareness campaigns and calorie-focused strategies, progress remains limited. Clinical interventions such as bariatric surgery and new pharmacological treatments have yielded some results in managing severe obesity. But those approaches sometimes fail to address the complexity of obesity, which is influenced by behavioral, social, and systemic factors.
A recent systematic review by Kempf et al., highlights that meal replacements substituting main meals with prepackaged, nutritionally complete products like powders, shakes, or soups, along with lifestyle interventions, are not inferior to pharmacotherapies in weight reduction and long-term glycemic control.
What is the EU doing to address this challenge?
The European Commission plans to launch an EU Cardiovascular Health Plan in Q4 2025 to address the growing burden of cardiovascular diseases, which cause 1.7 million deaths annually and cost the EU about €280 billion. Obesity, smoking, high blood pressure, excess alcohol consumption, unhealthy diet and physical inactivity, and genetic predisposition are some of the drivers of CVDs.
The EU initiative aims to prevent diseases, improve early detection and screening, enhance management and rehabilitation, leveraging digital health tools, AI, and the European Health Data Space for personalised care. It seeks to reduce health inequalities, address gender-specific risks, and support vulnerable groups while fostering research and innovation to close existing gaps.
The plan will complement Member States’ efforts and strengthen Europe’s health ecosystem and competitiveness in medical technology. This creates an opportunity to integrate food innovation into policy frameworks, supporting nutrient-rich products and lifestyle interventions that align with broader health goals.
Implications: Cost, Behavior, and Consumer Trends
Changing behavior demands sustained motivation, supportive environments, and practical tools that make healthy choices easier. Yet despite growing awareness, behavioral barriers persist: many individuals struggle to adopt healthier eating habits, and food choices remain driven by convenience and affordability.
Professor Adam Drewnowski, a globally recognized authority on diet quality and food economics, serves as Professor of Epidemiology and directs the Center for Public Health Nutrition at the University of Washington has described the challenge of aligning health, cost, and sustainability in food systems as an “impossible trinity.” His research underscores a critical truth: unless food systems are reoriented to deliver nutritious, affordable, and accessible options, sustainable change will remain out of reach. Policymakers must recognize that health-driven innovation in food is not a luxury – it’s a necessity for long-term resilience.
Why Are Current Strategies Falling Short?
Despite extensive research, obesity persists. People appear to struggle to eat healthy and nutritious food, live an active lifestyle and count calories. Furthermore, it does not account for differences in nutrient quality. Focusing solely on calories can lead to poor food choices—low-calorie but nutrient-poor options—whereas prioritising nutrient density ensures the body gets essential vitamins, minerals, and quality macronutrients for long-term health.
The work done by Al-Najim et al., under the Strive Study looked into outcomes of different lifestyle approaches to tackling obesity. This multicentre, open-label, realworld clinical trial evaluated the effectiveness of different interventions. One strand of the study focused on standard care to fight obesity and comparing it against diets involving nutrient-dense meal replacements—such as Herbalife’s Formula 1— with structured lifestyle support.
Over a period of two years, the standard care cohort showed a slight increase in weight while the meal replacement cohort lost an average of 5.7 kg, demonstrating that individuals can make lasting changes by addressing both nutritional quality and behavioral factors. Thus, meal replacement lifestyle interventions might be considered as valid approaches to curb the rise of obesity levels.
Professor Carel le Roux, Head of Metabolic Medicine at University College Dublin, and one of the authors of the study, said: “This study is further evidence of the effectiveness of using meal replacements to help treat the disease of obesity, particularly in those with more severe forms of the disease.”
Andrea Bertocco PhD, Senior Principal Scientist at Herbalife said: “With over 45 years’ experience developing best-in-class meal replacement shakes and nutritional supplements, we understand how difficult the challenge of weight loss can be. It’s fantastic to see the results of this study and just how beneficial meal replacement shakes can be when coupled with exercise and a reduction in calorie consumption.”
The Strive Study revealed significant weight loss and improvements in metabolic markers among participants, demonstrating the effectiveness of structured interventions. The findings provide strong evidence that regulated, nutrient-rich products can play a positive role in public health strategies.
Public discourse often focuses on food processing rather than nutritional value. The Dublin Weight Loss Clinical Trial underscores the need to prioritise nutrient density as a measure of healthiness. Herbalife’s approach demonstrates how regulated, nutrient-rich processed foods can support weight management and overall health.
As Europe shifts toward prevention-focused health systems, policymakers should recognise the role of innovative nutrition solutions in tackling obesity. It’s time to move beyond calorie counting and embrace strategies that make healthy living practical, affordable, and sustainable.
Don’t miss the opportunity to register to the topic-related Herbalife event on the 2nd of December HERE