Badhwar, A. et al. Assessment of brain-derived extracellular vesicle enrichment for blood biomarker analysis in age-related neurodegenerative diseases: an international overview. Alzheimers Dement 20, 4411–4422 (2024).
Gonzales M. M. et al. Biological aging processes underlying cognitive decline and neurodegenerative disease. J. Clin. Investig. 132. https://doi.org/10.1172/JCI158453 (2022).
Van Hove L. I. et al. Converging cross-modal evidence for a phylogenetic age effect in neurodegenerative susceptibility. Brain, published online Feb 5. https://doi.org/10.1093/brain/awaf050. (2025).
de Fátima Dias M., Duarte J. V., de Carvalho P., Castelo-Branco M. Unravelling pathological ageing with brain age gap estimation in Alzheimer’s disease, diabetes, and schizophrenia. Brain Commun. published online March 11. https://doi.org/10.1093/braincomms/fcaf109 (2025).
Hatos, A. Anxiety in the age of AI: constructing a tool to assess public perceptions. Brain 16, 415 (2025).
Yi, F. et al. Genetically supported targets and drug repurposing for brain aging: a systematic study in the UK Biobank. Sci. Adv. 11, eadr3757 (2025).
Bellantuono, L. et al. Predicting brain age with complex networks: from adolescence to adulthood. Neuroimage 225, 117458 (2021).
Hong, J. et al. Brain age prediction of children using routine brain MR images via deep learning. Front Neurol. 11, 584682 (2020).
Nemati, S., Arjmandi, M., Busby, N., Bonilha, L. & Fridriksson, J. The impact of age-related hearing loss on cognitive decline: the mediating role of brain age gap. Neuroscience 551, 185–195 (2024).
Teselink, J. et al. Efficacy of non-invasive brain stimulation on global cognition and neuropsychiatric symptoms in Alzheimer’s disease and mild cognitive impairment: a meta-analysis and systematic review. Ageing Res Rev. 72, 101499 (2021).
Tian, Y. E. et al. Heterogeneous aging across multiple organ systems and prediction of chronic disease and mortality. Nat. Med. 29, 1221–1231 (2023).
Ballester, P. L. et al. Gray matter volume drives the brain age gap in schizophrenia: a SHAP study. Schizophrenia 9, 3 (2023).
Siddiqi et al. Brain stimulation and brain lesions converge on common causal circuits in neuropsychiatric disease. Nat. Hum. Behav. 5, 1707–1716 (2021).
Almeida, F. C. et al. Lewy body co-pathology in Alzheimer’s disease and primary age-related tauopathy contributes to differential neuropathological, cognitive, and brain atrophy patterns. Alzheimers Dement 21, e14191 (2025).
Dinsdale, N. K. et al. Learning patterns of the ageing brain in MRI using deep convolutional networks. Neuroimage 224, 117401 (2021).
He, S., Feng, Y., Grant, P. E. & Ou, Y. Deep relation learning for regression and its application to brain age estimation. IEEE Trans. Med. Imaging 41, 2304–2317 (2022).
Cai, H., Gao, Y. & Liu, M. Graph transformer geometric learning of brain networks using multimodal MR images for brain age estimation. IEEE Trans. Med. Imaging 42, 456–466 (2023).
Honea, R. A. et al. TOMM40 may mediate GFAP, neurofilament light Protein, pTau181, and brain morphometry in aging. Aging Brain 7, 100134 (2025).
Hernandez, A. R. et al. Microbiome-driven alterations in metabolic pathways and impaired cognition in aged female TgF344-AD rats. Aging Brain 5, 100119 (2024).
Fadadu, R. P., Bozack, A. K. & Cardenas, A. Chemical and climatic environmental exposures and epigenetic aging: a systematic review. Environ. Res. 274, 121347 (2025).
Condello, G. et al. Energy balance and active lifestyle: potential mediators of health and quality of life perception in aging. Nutrients 11, 2122 (2019).
Ploughman, M., Wallack, E. M., Chatterjee, T., Kirkland, M. C. & Curtis, M. E. Health Lifestyle and Aging with MS Consortium. Under-treated depression negatively impacts lifestyle behaviors, participation and health-related quality of life among older people with multiple sclerosis. Mult. Scler. Relat. Disord. 40, 101919 (2020).
Zhang, X.-H., Huang, H.-W., Zeng, J.-Y., Chen, H.-J. & Lin, Y.-J. The beneficial influence of night-shift napping on brain core cognition networks in nurses experiencing sleep deprivation: A preliminary resting-state fMRI study. Sleep. Med. 131, 106503 (2025).
Zhang, R. et al. Associations of dietary patterns with brain health from behavioral, neuroimaging, biochemical and genetic analyses. Nat. Ment. Health 2, 535–552 (2024).
Tian Y. E., Cole J. H., Bullmore E. T., Zalesky A. Brain, lifestyle and environmental pathways linking physical and mental health. Nat. Ment. Health published online Aug 9. https://doi.org/10.1038/s44220-024-00303-4 (2024).
Seitz-Holland, J., Haas, S. S., Penzel, N., Reichenberg, A. & Pasternak, O. BrainAGE, brain health, and mental disorders: a systematic review. Neurosci. Biobehav Rev. 159, 105581 (2024).
Guo, J. et al. Mendelian randomization analyses support causal relationships between brain imaging-derived phenotypes and risk of psychiatric disorders. Nat. Neurosci. 25, 1519–1527 (2022).
Leonardsen, E. H. et al. Genetic architecture of brain age and its causal relations with brain and mental disorders. Mol. Psychiatry 28, 3111–3120 (2023).
Bravo-Ortiz, M. A. et al. A systematic review of vision transformers and convolutional neural networks for Alzheimer’s disease classification using 3D MRI images. Neural Comput. Appl. 36, 21985–22012 (2024).
Das B. K. et al. VIViT: variable-input vision transformer framework for 3D MR image segmentation. arXiv [eess.IV]. published online May 13. http://arxiv.org/abs/2505.08693 (2025).
Gibbon S., Breen D. P., MacGillivray T. J., UK Biobank Eye & Vision Consortium. Optic disc pallor in Parkinson’s disease: a UK Biobank study. Mov. Disord published online Jan 30. https://doi.org/10.1002/mds.30127 (2025).
Hanazawa, R., Sato, H. & Hirakawa, A. Alzheimer’s Disease Neuroimaging Initiative. Mixture disease progression model to predict and cluster the long-term trajectory of cognitive decline in Alzheimer’s disease. Ther. Innov. Regul. Sci. 59, 264–277 (2025).
Nudelman K. N. H., Brumm M. C., Marek K., Foroud T. M., for the Parkinson’s Progression Markers Initiative (PPMI) Study. TREM2 variants in Parkinson’s disease: results from the Parkinson’s progression markers initiative (PPMI) study. Alzheimers Dement. 18. https://doi.org/10.1002/alz.062316 (2022).
Giff, A. et al. Spatial normalization discrepancies between native and MNI152 brain template scans in gamma ventral capsulotomy patients. Psychiatry Res Neuroimaging 329, 111595 (2023).
Giff, A. et al. 19. Spatial normalization discrepancies between native and MNI152 brain template scans in gamma ventral capsulotomy patients. Biol. Psychiatry 93, S101–S102 (2023).
Shen Q., Xiao B., Mi H., Yu J., Xiao L. Adaptive learning filters–embedded vision transformer for pixel-level segmentation of low-light concrete cracks. J. Perform Constr. Facil 39. https://doi.org/10.1061/jpcfev.cfeng-4952 (2025).
Sadeghi B., Alesheikh A. A., Jafari A., Rezaie F. Performance evaluation of convolutional neural network and vision transformer models for groundwater potential mapping. J. Hydrol. 132840 (2025).
Kundu B., Khanal B., Simon R., Linte C. A. Assessing the performance of the DINOv2 self-supervised learning vision transformer model for the segmentation of the left atrium from MRI images. In: Rettmann M. E., Siewerdsen J. H., eds. Medical Imaging 2025: Image-Guided Procedures, Robotic Interventions, and Modeling. 19 (SPIE, 2025).
Beheshti, I., Mishra, S., Sone, D., Khanna, P. & Matsuda, H. T1-weighted MRI-driven brain age estimation in Alzheimer’s disease and Parkinson’s disease. Aging Dis. 11, 618–628 (2020).
Zuo, Q. et al. Associations of metabolic syndrome with cognitive function and dementia risk: Evidence from the UK Biobank cohort. Diab. Obes. Metab. 26, 6023–6033 (2024).
Schulz, C.-A., Weinhold, L., Schmid, M., Nöthen, M. M. & Nöthlings, U. Analysis of associations between dietary patterns, genetic disposition, and cognitive function in data from UK Biobank. Eur. J. Nutr. 62, 511–521 (2023).
Susetyo, B. & Fitrianto, A. Estimating missing panel data with regression and multivariate imputation by chained equations (MICE). CAUCHY 9, 94–105 (2024).
Austin, P. C. Graphical methods to illustrate the nature of the relation between a continuous variable and the outcome when using restricted cubic splines with a Cox proportional hazards model. Stat. Methods Med Res. 34, 277–285 (2025).
Erratum to “A dose-effect network meta-analysis model with application in antidepressants using restricted cubic splines.” Stat. Methods Med. Res. 33, NP1 (2024).
Fuh, C.-D., Kao, C.-L. M. & Pang, T. Kullback-Leibler divergence and Akaike information criterion in general hidden Markov models. IEEE Trans. Inf. Theory 70, 5888–5909 (2024).
Saumard, A. & Navarro, F. Finite sample improvement of Akaike’s information criterion. IEEE Trans. Inf. Theory 67, 6328–6343 (2021).
Xia, L., Nan, B. & Li, Y. Statistical inference for Cox proportional hazards models with a diverging number of covariates. Scand. Stat. Theory Appl. 50, 550–571 (2023).
Hahn, G. et al. Polygenic hazard score models for the prediction of Alzheimer’s free survival using the lasso for Cox’s proportional hazards model. Genet. Epidemiol. 49, e22581 (2025).
Liu, W., Leung, D. & Shao, Q.-M. Asymptotic false discovery control of the Benjamini-Hochberg procedure for pairwise comparisons. Sci. China Math. https://doi.org/10.1007/s11425-022-2241-y (2024).
Hepsomali, P. & Groeger, J. A. Diet, sleep, and mental health: insights from the UK Biobank study. Nutrients 13, 2573 (2021).
Huang, S.-Y. et al. Sleep, physical activity, sedentary behavior, and risk of incident dementia: a prospective cohort study of 431,924 UK Biobank participants. Mol. Psychiatry 27, 4343–4354 (2022).
Chudasama, Y. V. et al. Healthy lifestyle and life expectancy in people with multimorbidity in the UK Biobank: A longitudinal cohort study. PLoS Med. 17, e1003332 (2020).
Zhang, Y.-B. et al. Associations of healthy lifestyle and socioeconomic status with mortality and incident cardiovascular disease: two prospective cohort studies. BMJ 373, n604 (2021).
Rodriguez D., Sued M., Valdora M. A Kruskal-Wallis type test for functional data. Commun Stat. Simul. Comput. 1–15 (2025).
Yap, S. M., Dillon, M., Crowley, R. K. & McGuigan, C. Alemtuzumab-related thyroid disease in people with multiple sclerosis is associated with age and brainstem phenotype at disease onset. Mult. Scler. J. Exp. Transl. Clin. 6, 2055217320933928 (2020).
Sharma S., Dhakal S., Bhavsar M. Transfer learning for wildlife classification: Evaluating YOLOv8 against DenseNet, ResNet, and VGGNet on a custom dataset. arXiv [cs.CV]. published online July 10. http://arxiv.org/abs/2408.00002 (2024).
Arnob, A. S., Kausik, A. K., Islam, Z., Khan, R. & Bin Rashid, A. Comparative result analysis of cauliflower disease classification based on deep learning approach VGG16, inception v3, ResNet, and a custom CNN model. Hybrid. Adv. 10, 100440 (2025).
Lee, J. et al. Deep learning-based brain age prediction in normal aging and dementia. Nat. Aging 2, 412–424 (2022).
Poloni, K. M. & Ferrari, R. J. A deep ensemble hippocampal CNN model for brain age estimation applied to Alzheimer’s diagnosis. Expert Syst. Appl. 195, 116622 (2022).
Baecker, L., Garcia-Dias, R., Vieira, S., Scarpazza, C. & Mechelli, A. Machine learning for brain age prediction: Introduction to methods and clinical applications. EBioMedicine 72, 103600 (2021).
He, S., Grant, P. E. & Ou, Y. Global-local transformer for brain age estimation. IEEE Trans. Med. Imaging 41, 213–224 (2022).
Pilli, R., Goel, T., Murugan, R. & Tanveer, M. Brain age estimation using universum learning-based kernel random vector functional link regression network. Cogn. Comput. 16, 3186–3199 (2024).
Pilli, R., Goel, T. & Murugan, R. Unveiling Alzheimer’s disease through brain age estimation using multi-kernel regression network and magnetic resonance imaging. Comput. Methods Prog. Biomed. 261, 108617 (2025).
Liu, W. et al. Risk prediction of Alzheimer’s disease conversion in mild cognitive impaired population based on brain age estimation. IEEE Trans. Neural Syst. Rehabil. Eng. 31, 2468–2476 (2023).
Koohsari, S. et al. Relationships of in vivo brain norepinephrine transporter and age, BMI, and gender. Synapse 77, e22279 (2023).
Cadena, E. J., White, D. M., Kraguljac, N. V., Reid, M. A. & Lahti, A. C. Evaluation of fronto-striatal networks during cognitive control in unmedicated patients with schizophrenia and the effect of antipsychotic medication. NPJ Schizophr. 4, 8 (2018).
Averbeck, B. & O’Doherty, J. P. Reinforcement-learning in fronto-striatal circuits. Neuropsychopharmacology 47, 147–162 (2022).
Tang, Y., Yan, Y., Mao, J., Ni, J. & Qing, H. The hippocampus associated GABAergic neural network impairment in early-stage of Alzheimer’s disease. Ageing Res Rev. 86, 101865 (2023).
Pal, G. et al. Global cognitive function and processing speed are associated with gait and balance dysfunction in Parkinson’s disease. J. Neuroeng. Rehabil. 13, 94 (2016).
Ebaid, D., Crewther, S. G., MacCalman, K., Brown, A. & Crewther, D. P. Cognitive processing speed across the lifespan: beyond the influence of motor speed. Front. Aging Neurosci. 9, 62 (2017).
Albrecht, F. et al. Investigating underlying brain structures and influence of mild and subjective cognitive impairment on dual-task performance in people with Parkinson’s disease. Sci. Rep. 14, 9513 (2024).
Abd-Alrazaq, A., Ahmed, A., Alali, H., Aldardour, A. M. & Househ, M. The effectiveness of serious games on cognitive processing speed among older adults with cognitive impairment: systematic review and meta-analysis. JMIR Serious Games 10, e36754 (2022).
Liu, Y. et al. The interaction between ageing and Alzheimer’s disease: insights from the hallmarks of ageing. Transl. Neurodegener. 13, 7 (2024).
Bogdanova I. et al. The effectiveness of rehabilitation programs for the mobilization of compensatory-adaptive neuroplasticity processes in patients with Parkinson’s disease according to indicators of neurotrophic factors. Ukrains’kyi Visnyk Psykhonevrolohii 18–23 (2022).
Passaretti, M. et al. Neurophysiological markers of motor compensatory mechanisms in early Parkinson’s disease. Brain 147, 3714–3726 (2024).
Rademacher, K. & Nakamura, K. Role of dopamine neuron activity in Parkinson’s disease pathophysiology. Exp. Neurol. 373, 114645 (2024).
Yegorov, Y. E., Poznyak, A. V., Nikiforov, N. G., Sobenin, I. A. & Orekhov, A. N. The link between chronic stress and accelerated aging. Biomedicines 8, 198 (2020).
Bobba-Alves, N. et al. Cellular allostatic load is linked to increased energy expenditure and accelerated biological aging. Psychoneuroendocrinology 155, 106322 (2023).
Jamea, A. A. et al. Altered default mode network activity and cortical thickness as vulnerability indicators for SCZ: a preliminary resting state MRI study. Eur. Rev. Med. Pharm. Sci. 25, 669–677 (2021).
Wang, H. et al. Shared genetic architecture of cortical thickness alterations in major depressive disorder and schizophrenia. Prog. Neuropsychopharmacol. Biol. Psychiatry 135, 111121 (2024).
Klotz, L., Antel, J. & Kuhlmann, T. Inflammation in multiple sclerosis: consequences for remyelination and disease progression. Nat. Rev. Neurol. 19, 305–320 (2023).
Psenicka, M. W., Smith, B. C., Tinkey, R. A. & Williams, J. L. Connecting neuroinflammation and neurodegeneration in multiple sclerosis: Are oligodendrocyte precursor cells a nexus of disease?. Front Cell Neurosci. 15, 654284 (2021).
Nian, K., Harding, I. C., Herman, I. M. & Ebong, E. E. Blood-brain barrier damage in ischemic stroke and its regulation by endothelial mechanotransduction. Front. Physiol. 11, 605398 (2020).
Li, X. et al. Endothelial cells and the blood-brain barrier: Critical determinants of ineffective reperfusion in stroke. Eur. J. Neurosci. 61, e16663 (2025).
Sone, D. et al. Neuroimaging-based brain-age prediction in diverse forms of epilepsy: a signature of psychosis and beyond. Mol. Psychiatry 26, 825–834 (2021).
Hwang, G. et al. Brain aging in temporal lobe epilepsy: chronological, structural, and functional. NeuroImage Clin. 25, 102183 (2020).
Gong Y. et al. Progression of frailty and cardiovascular outcomes among Medicare beneficiaries. medRxiv 2024; published online Feb 13 https://doi.org/10.1101/2024.02.09.24302612 (2024).
Bernal J. et al. Longitudinal evidence for a mutually reinforcing relationship between white matter hyperintensities and cortical thickness in cognitively unimpaired older adults. medRxiv. published online July 10. https://doi.org/10.1101/2024.07.08.24309994 (2024).
Jiménez-Balado, J., Habeck, C., Stern, Y. & Eich, T. The relationship between cortical thickness and white matter hyperintensities in mid to late life. Neurobiol. Aging 141, 129–139 (2024).
Sanford N. et al Lifestyle and BrainAGE in adult depression. medRxiv. 2025; published online March 28. https://doi.org/10.1101/2025.03.27.25324698.
Turpin, A.-L. et al. Association between lifestyle at different life periods and brain integrity in older adults. Neurology 104, e213347 (2025).
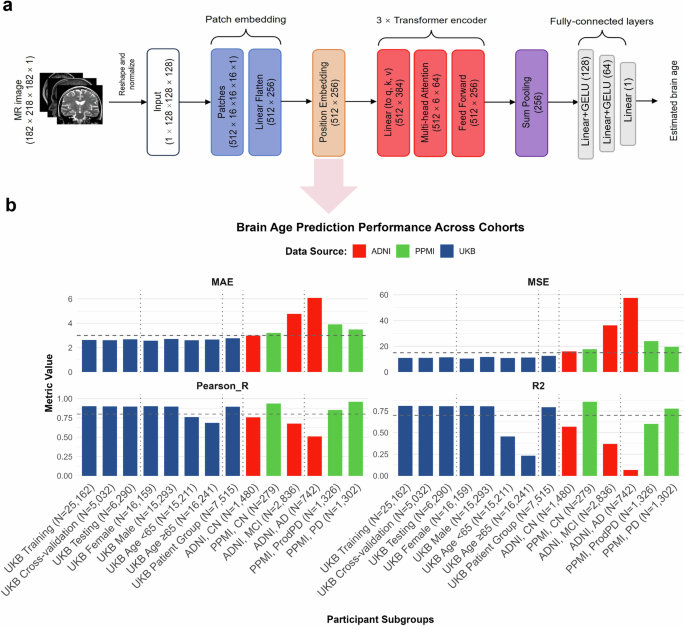
Zhang, R. & Yi, F. Brain age gap model. Zenodo https://doi.org/10.5281/zenodo.16159489 (2025).